The Model for Improvement – Quality Improvement – East London NHS Foundation Trust
The Model for Improvement
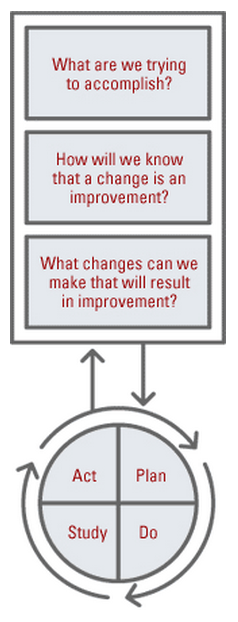
The ‘Model for Improvement’ is the framework we are using to drive continuous improvement.
It is essentially a method for structuring an improvement project. If you are looking to carry out a QI project, we will help guide you to develop your idea and test it out using this simple framework.
The model consists of two parts. The first three questions help us define what we want to achieve, what ideas we think might make a difference, and what we’ll measure to help us understand if change is an improvement.
The second part is the PDSA (Plan Do Study Act) cycle – outlining the steps for the actual testing of the change ideas. The cyclical nature allows the change to be refined and improved through repeated cycles of testing and learning. This provides a vehicle for continuous improvement.
Model for Improvement – Part 1 – The Framework
What are we trying to accomplish?
- Take the quality issue you’ve identified and turn it into an aim. Something that is SMART (Specific, Measurable, Achievable, Realistic, Timebound). We need to be able to say how good what it is we are improving is and by when. That way we’ll be able to show whether our quality improvement project is working.
Model for Improvement – Part 2 – The Engine
How will we know that a change is an improvement?
- We all measure things in our day to day jobs and in quality improvement this is no different. There are 3 types of measures we use in improvement projects:
Outcome – This is often directly linked to your aim e.g If your QI project was focusing on falls reduction then your outcome measure could be the number of falls occurring. There is often a tangible link between the outcome measure and the service user/end user.
Process -Your improvement project will likely involve changing or modifying different processes or systems to hopefully improve the quality issue you’ve identified. Its important to measure the reliability of these processes so you can track them back against your aim. For example going back to your falls project, you may want to focus on the process of risk assessment which will then help reduce the number of falls.
Balance – These can help show whether unintended consequences have been introduced elsewhere in the system
More about measures
Outcome Measures
How does the system impact the values of patients, their health and wellbeing? What are impacts on other stakeholders such as payers, employees, or the community?
- For diabetes: Average hemoglobin A1c level for population of patients with diabetes
- For access: Number of days to 3rd next available appointment
- For critical care: Intensive Care Unit (ICU) percent unadjusted mortality
- For medication systems: Adverse drug events per 1,000 doses
Process Measures
Are the parts/steps in the system performing as planned? Are we on track in our efforts to
improve the system?
- For diabetes: Percentage of patients whose hemoglobin A1c level was measured twice in the past year
- For access: Average daily clinician hours available for appointments
- For critical care: Percent of patients with intentional rounding completed on schedule.
Balancing Measures
(looking at a system from different directions/dimensions)
Are changes designed to improve one part of the system causing new problems in other parts of the system?
- For reducing time patients spend on a ventilator after surgery: Make sure reintubation rates are not increasing
- For reducing patients’ length of stay in the hospital: Make sure readmission rates are not increasing
For every project you will need between 5-8 measures.
What changes can we make that result in improvement? In order to improve quality we’ll need to make changes, though not every change will result in improvement. One way of trying to think about changes and also to understand the system in which you are working in is to use a driver diagram.

For more details about the model for improvement, visit the IHI website.






